Daylight Saving Time May Increase Risks Of Heart Attacks
While daylight saving time might appear like a great way to save energy, research has not shown any clear results. In fact, it actually has more negative consequences than benefits. Recent studies have highlighted that clock changes increases the risk of heart attacks. Slight sleep deprivation triggered by this time shift causes circadian misalignment, which increases the heart attack risks by almost 30%.
Clock Change Causes Heart Attacks
A recent paper1Manfredini, R., Fabbian, F., Cappadona, R. et al. Intern Emerg Med (2018) 13: 641. https://doi.org/10.1007/s11739-018-1900-4 written by the Universities of Ferrara and Florence in Italy, warned of the risk of biannual clock change, particularly during the first week of the time change. According to the paper, for the majority of individuals, the tiredness caused by time change might seem like a small issue but for others, it can result in graver consequence.
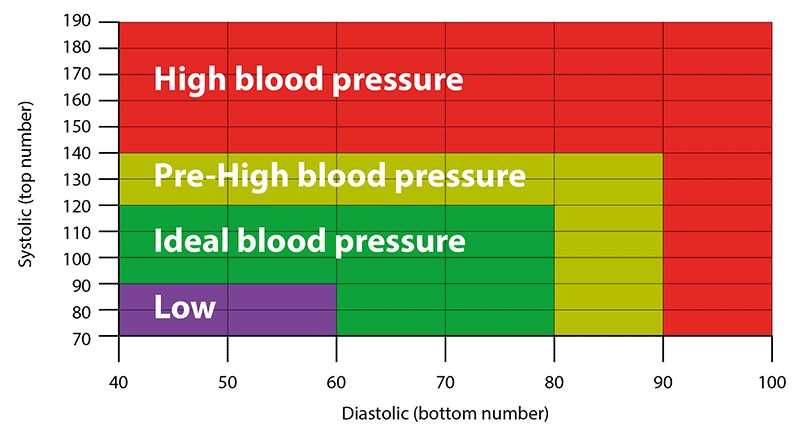
Studies have highlighted the link between heart attacks and lack of sleep. Less than six hours of sleep is associated with obesity, diabetes, blood pressure, and premature death. Disrupted sleep leads to consumption of more calories and fewer calories burned. Moreover, just one sleepless night is enough to enhance insulin resistance.
The research reviewed existing heart attacks and daylight saving time literature and found that the Monday after the time change has the most number of heart attacks. The first day of the week is also a critical one for Takotsubo cardiomyopathy, also referred to as “broken heart syndrome”. This is a condition where the heart muscle suffers a temporary and sudden weakness, which is caused due to emotional stress, increased blood pressure, and higher levels of catecholamine, the fight-or-flight hormones.
What’s the Reason?
Human bodies prefer a longer day as compared to a shorter day. The research referred to travelling numerous time zones, which cause the worse possible jet lag. The same pattern has been associated with daylight time change transitions.
The circadian rhythm of the human body controls the sense of night and day, time to sleep, eat and more. The same rhythm helps in regulating the metabolism to body organs, including the heart. The change in time causes an imbalance in your body clock, especially in sensitive people. Merely an hour of lost sleep might enhance stress levels, blood pressure, heart rate, as well as chemicals promoting inflammation.
Other Consequences of Daylight Saving Time
Another study2American Academy of Neurology (AAN). “Does daylight saving time increase risk of stroke?.” ScienceDaily. ScienceDaily, 29 February 2016. www.sciencedaily.com/releases/2016/02/160229220653.htm presented at the American Academy of Neurology’s 68th Annual Meeting in Vancouver, Canada, April 15 – 21, 2016, found that there is an 8% increase in cases of ischemic stroke in the first two days of daylight clock change as compared to the two weeks before and two weeks after the time change.The Universities of Washington and Virginia published a study3Cho, K., Barnes, C. M., & Guanara, C. L. (2017). Sleepy Punishers Are Harsh Punishers: Daylight Saving Time and Legal Sentences. Psychological Science, 28(2), 242–247. https://doi.org/10.1177/0956797616678437 which highlighted that the Monday after the daylight saving time switch, the legal sentences given out in courts were 5% longer as compared to the previous Monday and the following Monday. This indicated that the time switch affected their sleep, making the judges less productive.
This was supported by research4Wagner, D. T., Barnes, C. M., Lim, V. K. G., & Ferris, D. L. (2012). Lost sleep and cyberloafing: Evidence from the laboratory and a daylight saving time quasi-experiment. Journal of Applied Psychology, 97(5), 1068-1076 http://dx.doi.org/10.1037/a0027557. published in the Journal of Applied Psychology, stating that this time switch promotes productivity-draining endeavors, referred to as cyberloafing (surfing the net, checking personal emails on work time). The same was true for undergraduate students who were found to engage in cyberloafing 8.4 minutes more than usual after time switch.
While all these results have been observational, they strongly indicate that daylight saving time is causing more harm than benefits. The research highlighted that merely one day (Sunday), is not enough time for people to get accustomed to the time switch, making it harder on them for the rest of the week.