New Guidance For Hypertension Consultation
The National Institute for Health and Care Excellence (NICE) has made a major change in the blood pressure guidance last published in 20111 Hypertension in adults: diagnosis and management – National Institute for Health and Care Excellence (NICE) . The draft guidelines 2 Hypertension in adults: diagnosis and management, Draft for consultation, March 2019 – National Institute for Health and Care Excellence (NICE) recommend the threshold of hypertension treatment should be reduced, which makes more than 450,000 men and 270,000 women eligible for blood pressure treatment. This means that an increased number of individuals would be offered drugs to lower blood pressure as a means to prevent strokes and heart attacks. This guidance has been released for consultation till April, 30 and is expected to be finalized by August 2019.
Previous Guidelines and New Recommendations
According to the NICE recommended guidance from 2011, drugs for lowering blood pressure should be given to individuals under 80 years of age who are suffering from stage one hypertension and are at 20% or more risk of cardiovascular disease in the next ten years.
As per the new recommendations, NICE has recommended offering blood pressure lowering drugs to patients with 10% or more risk of cardiovascular disease.
Stage one hypertension is when there isn’t any identifiable reason behind the increase in blood pressure. It might be associated with different factors, including genetics, physical activity, salt intake, or obesity.
According to the guideline committee chairman, Anthony Wierzbicki 3 Thousands set to benefit from blood pressure treatment under new NICE guidance – National Institute for Health and Care Excellence (NICE) , these changes in the guidelines have resulted in updating the previous recommendations for early intervention of hypertension and is expected to make major differences in the lives of patients suffering from this condition.
The Reason
The recommended new guidelines will shift the focus effectively towards early intervention with either drug treatment or lifestyle treatment. The aim is to reduce the age-related blood pressure issues and help patients live a longer life with reduced need for consuming multiple drugs.
Hypertension is one of the leading causes of strokes and heart attacks in the country, but countless individuals are not undiagnosed.
The early diagnosis of blood pressure will result in earlier treatment and prevention as per the NICE recommended guidelines, which will save the lives of thousands while also enhancing the quality of their lives. This is the aim of the new changes in the guidelines and to enhance the management and detection of high blood pressure in the next ten years.
Taking these steps for preventing cardiovascular disease is an important step to safeguard their long-term well-being and health.
Concerns Regarding New Recommendations
While these new guidelines will help with the early detection, many experts have raised concerns about unintended harm and over-diagnosis issues of offering prescribed medications to patients when the advantages might be restricted.
They believe that to lower the threshold of hypertension diagnosis, which is a condition that affects a major number of individuals in the country, it is essential to ensure that this decision is evidence-based and not taken lightly.
A major chunk of the population is already suffering from undiagnosed hypertension, which means they are at high risk of a deadly stroke or heart attack. Therefore, it is essential to enhance the diagnosis around the country, but it is also important to make sure that the changes will actually improve the quality of lives of the patients and not put them at more risk.











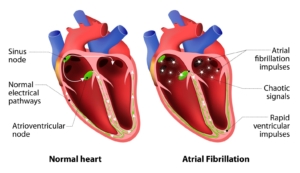
 AF-related strokes cause unacceptably high levels of death and disability, and the scale of the problem across Europe is increasing as our populations age.
AF-related strokes cause unacceptably high levels of death and disability, and the scale of the problem across Europe is increasing as our populations age.
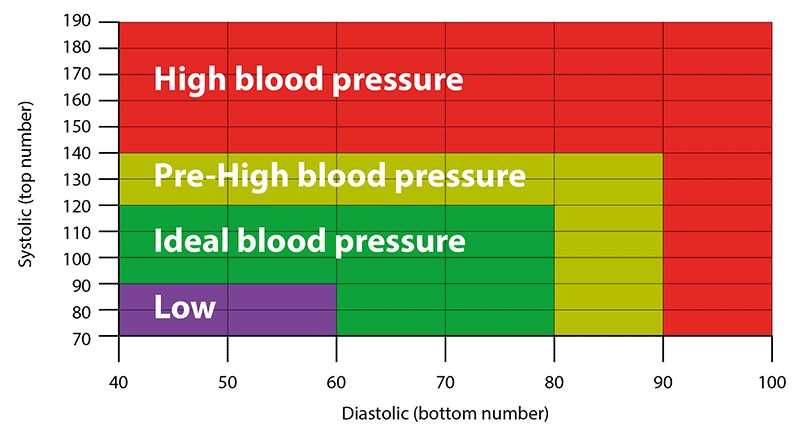
 Ambulatory Blood Pressure Monitors (ABPMs) provide testing to determine the presence of hypertension by taking measurements during normal daily activities, over a span of 24 (or more) hours. They help to diagnose as well as monitor high blood pressure (hypertension), usually defined as a systolic pressure of 140 mm Hg or more and a diastolic pressure of 90 mm Hg or more.
Ambulatory Blood Pressure Monitors (ABPMs) provide testing to determine the presence of hypertension by taking measurements during normal daily activities, over a span of 24 (or more) hours. They help to diagnose as well as monitor high blood pressure (hypertension), usually defined as a systolic pressure of 140 mm Hg or more and a diastolic pressure of 90 mm Hg or more.